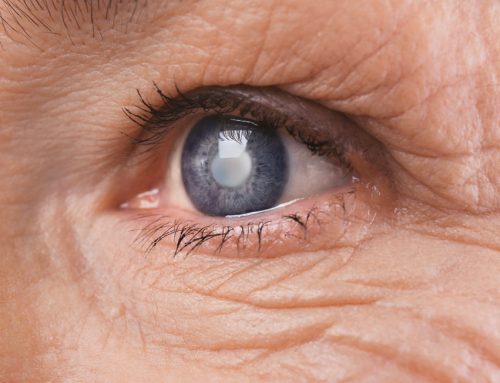
If you have diabetes, regular eye examinations are important to detect and treat eye problems. These should be arranged by your diabetes health team as part of regular tests and screening. High blood sugar (glucose) increases the risk of diabetes eye problems. In fact, diabetes is the leading cause of blindness in adults aged 20 to 74. Blurred vision can be a symptom of more serious eye problems with diabetes. The three major eye problems that people with diabetes may develop and should be aware of are cataracts, glaucoma, and retinopathy.
Diabetic retinopathy
The retina contains a group of specialised cells that convert light as it enters though the lens into visual signals. The eye nerve or optic nerve transmits visual information to the brain. Diabetic retinopathy is one of the vascular (blood-vessel related) complications related to diabetes. This diabetes eye problem is due to damage of small vessels and is called a “microvascular complication.” Kidney disease and nerve damage due to diabetes are also microvascular complications. Large blood vessel damage (also called macrovascular complications) includes complications like heart disease and stroke.
The microvascular complications have, in numerous studies, been shown to be related to high blood sugar levels. You can reduce your risk of these eye-related diabetes complications by improving your blood sugar control.
Diabetic retinopathy is the leading cause of irreversible blindness in industrialised nations. The duration of diabetes is the single most important risk for developing retinopathy. So the longer you have diabetes, the greater the risk of this very serious eye problem. If retinopathy is not found early or is not treated, it can lead to blindness.
People with type 1 diabetes rarely develop retinopathy before puberty. In adults with type 1 diabetes, it is also rare to see retinopathy before five years’ duration of diabetes. The risks of retinal damage increase with progressive duration of diabetes.
Intensive control of blood sugar levels will reduce your risks of developing retinopathy. The Diabetes Control and Complications Trial, a large study of people with type 1 diabetes, showed that people with diabetes who achieved tight control of their blood sugars with either an insulin pump or multiple daily injections of insulin were 50%-75% less likely to develop retinopathy, nephropathy (kidney disease), or nerve damage (all microvascular complications).
People with type 2 diabetes often have signs of eye problems when diabetes is diagnosed. In this case, control of blood sugar, blood pressure, and blood cholesterol have an important role in slowing the progression of retinopathy and other eye problems.
Types of retinopathy in diabetes:
• Background retinopathy. Sometimes the blood vessel damage exists, but there is no vision problem. This is called background retinopathy. It’s important to carefully manage your diabetes at this stage to prevent background retinopathy from progressing to more serious eye disease.
• Maculopathy. In maculopathy, the person has developed damage in a critical area called the macula. Because this occurs in an area that is critical to vision, this type of eye problem can significantly reduce vision.
• Proliferative retinopathy. New blood vessels start to grow in the back of the eye. Because retinopathy is a microvascular complication of diabetes, a disease of small vessels, this type of retinopathy develops because of an increasing lack of oxygen to the eye from vascular disease. Vessels in the eye are thinned and occluded and they start to remodel.
Here, it is important to address the risks factors that can worsen the occluded vessels. Smoking cessation, high blood pressure control, cholesterol management, and blood sugar control must take place in order to stop the damage to blood vessels and progression of new vessels from growing into the eye. These are fragile vessels that can bleed and eventually cause a clot to form in the retina, which scars and may cause detachment of the retina. This can eventually lead to irreversible vision loss.
Treatment of diabetic retinopathy may involve laser procedures or surgery. In a study of people with diabetes with early retinopathy, laser therapy to burn the fragile vessel resulted in a 50% reduction of blindness.
To prevent damage from retinopathy it’s important to have eye screening annually, or more frequently if recommended. Women with diabetes who later become pregnant should have a comprehensive eye examination during the first trimester and close follow-up with an eye specialist during the rest of their pregnancy to avoid serious eye problems with diabetes. (This recommendation does not apply to women who develop gestational diabetes, since they are not at risk of retinopathy.)
When to seek medical advice about eye problems in diabetes
If you have diabetes, seek medical advice about any eye problems if any of the following occur:
• Black spots in your vision.
• Flashes of light.
• “Holes” in your vision.
• Blurred vision.
Eye care for people with diabetes
Eye care is especially important for people with diabetes because they are at increased risk of developing eye complications from the disease. Retinopathy (damage to the retina at the back of the eye) is a common complication of diabetes. If left untreated, it can get worse and cause some loss of vision, or blindness in severe cases. All people with diabetes should take precautions to help reduce their risk of developing eye problems. Here are some eye care tips:
• Book regular appointments with your optometrist so that any eye problem can be detected early and treated
• Maintain control of your blood glucose levels
• Keep your blood pressure under control. High blood pressure by itself can lead to eye disease, so if you have high blood pressure as well as diabetes, it is especially important that you take steps to control both conditions
• Get your blood cholesterol levels under control
• Eat a healthy diet
• Avoid smoking
• Exercise regularly